COPD – Chronic obstructive pulmonary disease
Also known as emphysema or chronic bronchitis. There is currently no cure although there are treatments to help ease symptoms.
What is COPD?
COPD is an umbrella term for conditions where the airflow in the lungs is obstructed as a result of chronic and severe inflammation. This inflammation changes the small structure in the lungs leading to limited airflow in the lungs which worsened over time. Development of COPD occurs over many years mostly occurring in people aged 45 and over.
What are the different types of the condition?
The COPD term covers the following conditions:
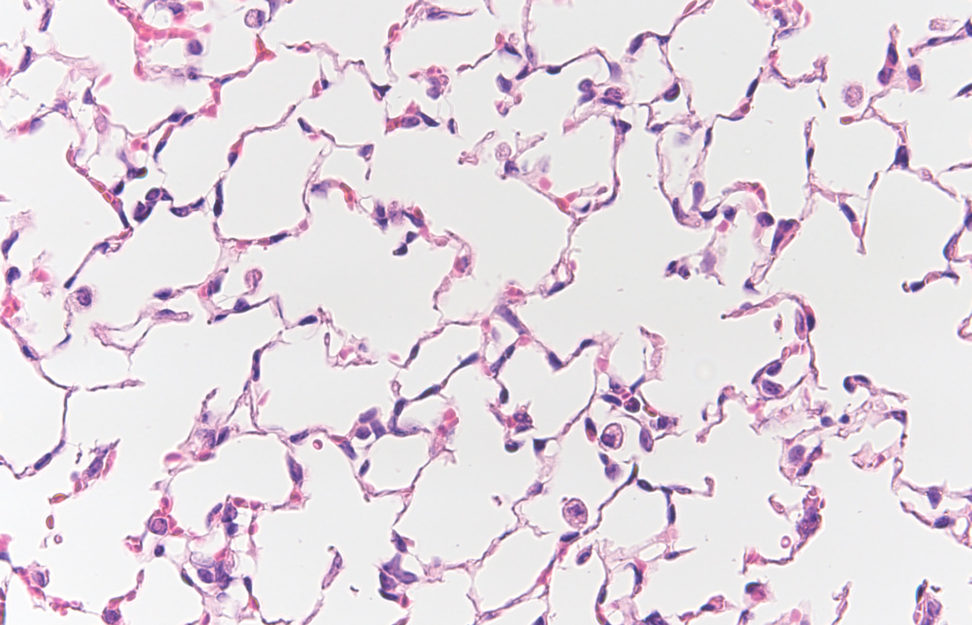
- Emphysema: tiny air sacs at the end of the airways in the lungs are destroyed
- Chronic bronchitis: a chronic cough resulting from inflammation in the airways
Who is at risk?
Major risk factors are long-term exposure to inhaled irritants in the environment. Critically, there is increasing evidence that ageing of the lung is accelerated. That is, that age associated changes in the structure and function of the lung are important in the disease’s development and progression.
Risk factors for COPD include:
- Exposure to tobacco smoke
- People with asthma
- Occupational exposure to dusts and chemicals
- Exposure to burning fuel and fumes
- Genetics
What are the symptoms of COPD?
Defined by abnormal lung function, a clinical test called ‘spirometry’ is required to accurately diagnose it. This test will identify if a person has trouble exhaling because their lungs are obstructed.
The COPD symptoms may include:
- Shortness of breath, especially during physical activities
- Wheezing
- Chest tightness
- Cough that may produce mucus
- Frequent respiratory infections
- Lack of energy
- Unexplained weight loss (in later stages)
- Swelling in ankles, feet or legs
Symptoms often don’t appear until significant lung damage has occurred, which usually worsens over time.
How is it treated?
Medications are used to reduce symptoms and complications in people with COPD. However there is no cure for the disease, only treatments that ease symptoms.
The role of research
Our researchers are looking at multiple ways to find new treatments for COPD. By understanding how the body works. They can see the fundamental mechanisms which are causing or affected by the disease.
We are looking at how the body’s metabolism manages inflammation and the immune response. While the lungs are the main organ affected, we are looking at how other organs such as the gut impact the progression of COPD. We are also looking at the genetic and epigenetic factors unique in COPD.
Inflammation in COPD
At Centenary, research into COPD is led by Professor Phil Hansbro, Director of the Centenary UTS Centre for Inflammation. He is looking at the impact of inflammation and potential treatments for COPD across multiple areas. These include fibrotic tissue remodelling, molecular impacts of infections and oxidative stress on the lungs.
The gut lung axis
Professor Hansbro’s recent findings also suggest a link between COPD and the gut microbiome and its metabolites. The ‘microbiome’ describes all of the microbes, particularly bacteria that exist in an individual.
His work suggests that an unhealthy or altered microbiome could be responsible for promoting inflammatory diseases such as COPD. The team is now aiming to determine the role and potential for modulating the gut microbiome and their products as potential new therapies.
Complications
Patients often experience complications such as:
- Respiratory infections: colds, the flu and pneumonia are more common and cause further damage to lung tissue.
- Heart problems: while not fully understood, an increase risk of heart disease is found in patients
- Lung cancer: a higher risk of developing lung cancer.
- High blood pressure in lung arteries: the arteries that bring blood to your lungs are affected by pulmonary hypertension.
- Depression: dealing with serious illness can contribute to the development of depression
Our research
At Centenary, we are committed to understanding COPD and other respiratory diseases. There is no current cure for COPD and patients often have poor outcomes. We believe by looking at the drivers of inflammation we can unlock potential treatments.
Our work includes projects that look at the effects of inflammation, molecular impacts of infections and oxidative stress. The epigenetic changes and fibrotic tissue remodelling on the airways and lungs and the role of our diet and microbiome.
Professor Phil Hansbro, Director of the Centenary UTS Centre for Inflammation leads this research.
Inflammation is a critical driver of many disease features of COPD including fibrosis, emphysema, impaired gas exchange and severe breathing difficulties. There are many different processes that contribute to inflammation (inflammatory epithelial cells, macrophages, mast cells, complement system, inflammasomes) that we have high level expertise in. We have specific tools that we can use to define their specific roles and which are most important in driving COPD.
These processes are major drivers of disease pathology in COPD and other chronic respiratory diseases. We have several new compounds, some naturally derived, that target and suppress these factors at their source. This source is damaged mitochondria that become dysfunctional when exposed to cigarette and bushfire smoke, air pollution and other environmental challenges.
We are analysing the microbial populations (the microbiome) and the factors that they produce (metabolites) in the lung and the gut. The research looks at how the microbiome drives or protects against COPD.
We are also looking at how these results can be modified with specific dietary components.
This is the study of processes that modify DNA without affecting its sequence. We are working out how these change in COPD (microRNA, acetylation, methylation) and how they change the activity of diseases and drive disease features.
Fibrosis is the deposition of collagen in lung tissue leading to hardening and damage of the airways and alveoli. It is a major feature of COPD but current therapies have little effect against it. We have advanced knowledge of the role of inflammation and how it drives fibrosis in the lung.
We are performing several studies where we perform high throughput analysis of different groups of factors (mRNA, microRNA, proteins, phosphoproteins, lipids, microbiomes, metabolomes, acetylation, methylation). We can integrate all of these analyses together to obtain a more holistic view of how COPD develops and progresses, and we can also identify pivotal factors that control different parts of the disease and may be more effective targets.
We can use our expertise in each of these areas to develop new therapies to prevent or reverse the development of disease features in COPD and other related diseases such as asthma, pulmonary fibrosis, COVID-19 and lung cancer.
Professor Phil Hansbro, Director of the Centenary UTS Centre for Inflammation leads this research.
This page was last reviewed by a Centenary researcher on 9 December, 2022.
Inflammation is a critical driver of many disease features of COPD including fibrosis, emphysema, impaired gas exchange and severe breathing difficulties. There are many different processes that contribute to inflammation (inflammatory epithelial cells, macrophages, mast cells, complement system, inflammasomes) that we have high level expertise in. We have specific tools that we can use to define their specific roles and which are most important in driving COPD.
These processes are major drivers of disease pathology in COPD and other chronic respiratory diseases. We have several new compounds, some naturally derived, that target and suppress these factors at their source. This source is damaged mitochondria that become dysfunctional when exposed to cigarette and bushfire smoke, air pollution and other environmental challenges.
We are analysing the microbial populations (the microbiome) and the factors that they produce (metabolites) in the lung and the gut. The research looks at how the microbiome drives or protects against COPD.
We are also looking at how these results can be modified with specific dietary components.
This is the study of processes that modify DNA without affecting its sequence. We are working out how these change in COPD (microRNA, acetylation, methylation) and how they change the activity of diseases and drive disease features.
Fibrosis is the deposition of collagen in lung tissue leading to hardening and damage of the airways and alveoli. It is a major feature of COPD but current therapies have little effect against it. We have advanced knowledge of the role of inflammation and how it drives fibrosis in the lung.
We are performing several studies where we perform high throughput analysis of different groups of factors (mRNA, microRNA, proteins, phosphoproteins, lipids, microbiomes, metabolomes, acetylation, methylation). We can integrate all of these analyses together to obtain a more holistic view of how COPD develops and progresses, and we can also identify pivotal factors that control different parts of the disease and may be more effective targets.
We can use our expertise in each of these areas to develop new therapies to prevent or reverse the development of disease features in COPD and other related diseases such as asthma, pulmonary fibrosis, COVID-19 and lung cancer.
Professor Phil Hansbro, Director of the Centenary UTS Centre for Inflammation leads this research.

